I just wrapped up the first week of my very first hospital rotation; and quite frankly, I feel much better about it now than I did a week ago. Antibiotic is my Achilles’ heel. I have a mental block—in one ear and out the other—when it comes to retaining antibiotics. There are just so many! It is hard as it is just to remember the generics and sometimes multiple brands associated with each. Then there are also the spectrums of activity, numerous indications, multiple generations within each class, toxicities, renal dosing, hepatic dosing, IV to PO conversions, resistance, so on and so forth.
My preceptor seems to have mind-reading abilities and offered me a week to brush up on my antimicrobials before allowing me to accompany him on his daily rounding routines on the floors. I spent a few days digging up lecture notes and searching the internet, but failed to find anything particularly useful. So I took it upon myself to create cheat sheets—personal reference guides. Above all, I find them particularly useful and hope that it will also aid you with your reviews.
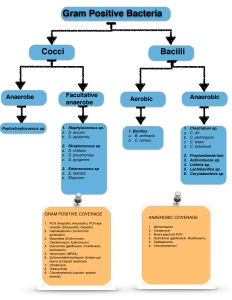
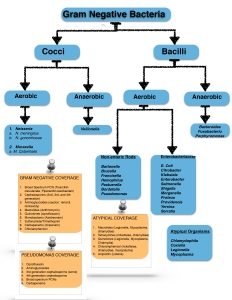
I began with the basics—identifying the culprit—the microorganisms. There are too many to possibly remember; therefore, it was helpful to group them into their groups of similar characteristic traits. The more we understand about these bacteria, the better chance we have at stopping them before they become deadly or cause serious harm.
One of my few first tasks on hospital rotation, I was to review patient’s microbiology lab results and match them up with the patient’s antibiotics regimen— a process in performing antibiotic therapy interventions. In order to correctly interpret culture results given to me, there were a few things I had to re-learn.Microbiology cultures are collect at different sites and sources, depending on the patient’s signs and symptoms upon admission. Microbiology data may include cultures collected in the blood, respiratory/sputum, stool, tissue, and urine. For example, if bacteremia was suspected, both central and peripheral blood cultures are to be collected and reviewed to confirm such diagnose. CFUs (colony-forming units), an estimate of number of viable bacteria cells in a sample, are extremely important in determine empiric therapy. In UTI for example, the magic number for is >100,000 CFUs. In some cases, asymptomatic UTI patients with CFU < 100,000 will not require antimicrobial therapy. Fluid hydration and bed rest may just be the best option.
Subsequent, culture sensitivity also plays a significant role in antimicrobial selection in institutional settings. For instance, Streptococcus pneumoniae culture for one pneumonia patient may generate a different list antibiotic sensitivity from another patient. After you have identified susceptibility, cost will be your next most influential factor. I recommend to get your hands on the institution’s antibiogram as soon as you can. Antibiograms are institution’s local susceptibility and resistance trends of antimicrobials, which can aid clinicians in choosing appropriate antimicrobial therapies. For example, Enterococcus faecalis is becoming resistant to ciprofloxacin at an alarming rate in patients with complicated UTIs. In situations like this, you may have to consider the use of ampicillin/sulbactam.
Other useful biology labs to be familiar with are antigen detection, PCR (polymerase chain reaction), and toxin detection. Antigen detection in sputum and pleural fluid can be used to rapidly identify CAP etiology, resulting in quickly identifying patients who are eligible for narrow spectrum antibiotics. PCR is the one of the most common approaches in diagnosing and characterization of bacterial meningitis. In addition, toxin detection is commonly used to detect Clostridium difficile colitis —responsible for antibiotic associated diarrhea— before discharge in patients previously on fluoroquinolones, cephalosporins, carbapenems, and clindamycin.
The topics in the next few blogs will involve my thought process—my methods and silly mnemonics— in the selection of appropriate antimicrobials based on microbiology cultures and lab results.



Thanks interesting read.
LikeLiked by 1 person
thanks!
LikeLike